MP SPEAKS | 10 questions for the Health DG
MP SPEAKS | Two days ago, on Jan 16, 2021, Malaysia reached a new high of 4,029 Covid-19 cases. We have just started the first week of the second movement control order (MCO 2.0), and this will go on for two weeks from Jan 13 until Jan 26. By contrast, we reached a high of 235 Covid-19 cases on March 26, 2020, during the first MCO.
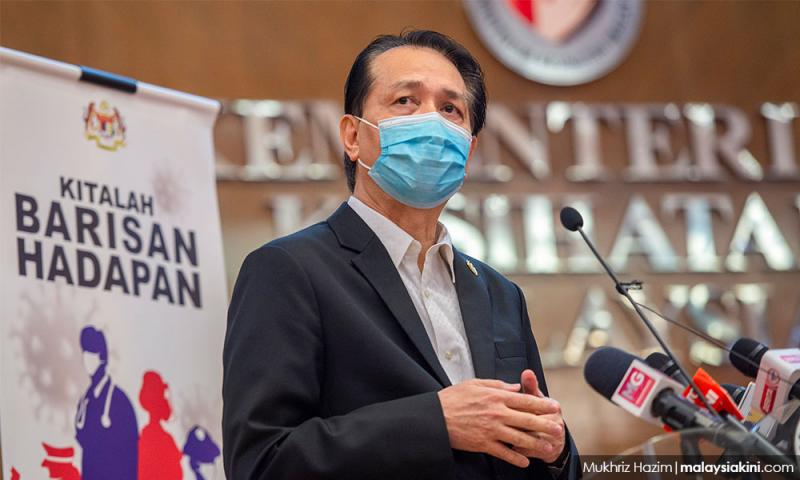
Credit should be given to the leadership of Health director-general Dr Noor Hisham Abdullah and the public health frontliners for their tireless efforts in combating the Covid-19 pandemic. But nine months after the first MCO, there are a number of questions which remain unanswered in our fight against the Covid pandemic.
I hope that DG Noor Hisham can provide convincing answers to the following 10 questions in order to assure the public that the government has a comprehensive plan to control this pandemic.
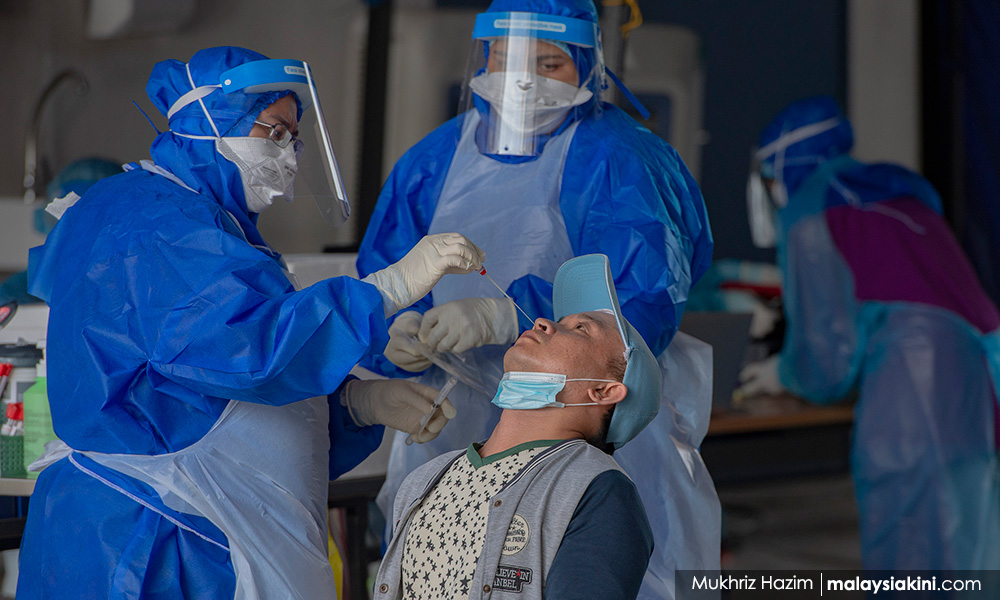
Q1: What is the total number of daily Covid-19 tests done by the Ministry of Health (MOH) and what is the daily percent of positive cases?
The daily focus has primarily been on the total number of new daily Covid-19 cases. While this number is important, we also need to know the total number of tests which are being done on a daily basis and the percent of positive cases.
This will give us an indication of (i) our testing capacity and (ii) the daily infection rate. According to a report in October 2020, Malaysia’s daily testing capacity then was approximately 54,000 but the average number of tests done was less than half this number.
If the daily testing capacity cannot be reached because of human resource shortages, the private sector (which is already doing their own tests) can be roped in to address this gap. Daily testing by the state will also be able to show shortages in the number of test kits in places like Sabah, for example.
Knowing the daily infection rate is also a useful indicator of infection trends moving forward. There have been many calls for the DG to make known the daily testing figures but until now, for reasons unknown, this figure has not been disclosed daily.
Q2: What is the number of contact tracers used by the Ministry of Health (MOH)? What measures have been put in place to address shortfalls in contact tracers?
As the number of daily cases spiked to more than 1,000, it was not surprising that the contact tracers would be overwhelmed. Over the past few weeks, reports had surfaced on how some families who have tested positive for Covid-19 had to wait for days before someone from MOH contacted them.
Earlier this month, my colleague and former deputy health minister, Dr Lee Boon Chye, asked for an additional 10,000 contact tracers to be hired on a temporary basis to deal with the spike in the number of Covi-19 cases.
There has been little disclosure on the number of contact tracers used by the MOH and even less discussion on the need to hire more contact tracers by the government.
Without a proper contact tracing infrastructure, our ability to contain this pandemic even after the end of MCO 2.0 will remain in question.
Q3: Can more accurate location information about Covid-19 cases be disclosed publicly?
To date, the MOH has been very reluctant to provide more accurate location information for new Covid-19 cases.
According to official reasoning, the government doesn’t want to cause a public panic in places where positive Covid-19 cases have been identified. But at the same time, the DG has been asking the public to avoid crowded places.
A more transparent and effective strategy would be for more accurate location information to be provided to the public so that they can stay informed. Without any official confirmation, unnecessary speculation about the exact location of new cases cannot be prevented.
New sites such as Malaysiakini already provide a daily report of places with new Covid-19 cases, but MOH does not verify this list. More transparent sharing of data would enable the public to make more well-informed choices about where to visit and where not to visit, especially after the end of MCO 2.0.
Q4: What transmission trends can be analysed based on MySejahtera data?
As of Nov 19, 2020, the Ministry of Health has recorded 1.7 billion check-ins by users via the MySejahtera app (with an average of 15 million daily check-ins) including for those Covid-19 positive patients.
Until now, we are not aware of whether this massive database has been analysed for transmission trends. For example, are the transmission rates higher in certain places such as gyms and restaurants compared to optometrists and hair salons? Once a factory cluster has been identified, what transmission mechanisms are most likely to cause community spread in the affected area?
We need to know this analysis to determine which businesses should be allowed to open during an MCO. We also need this information in order to improve and enhance our existing standard operating procedures (SOPs) to reduce transmission rates.
As of now, nobody is quite sure if, and how, the data from the MySejahtera application is being analysed and processed. This is one of the reasons why, for example, there is still uncertainty as to whether hair salons and optometrists should be allowed to operate during MCO 2.0.

Q5: What is the capacity in terms of the number of beds available and the intensive care unit (ICU) capacity by state?
To date, there has not been daily data released to show the capacity of beds available for Covid-19 patients as well as the total ICU capacity.
Ideally, this information should be given by state so that there is public transparency over existing hospital capacity and what additional steps need to be done to address shortages in this capacity. This would include the need to rope in private healthcare facilities to take in Covid-19 patients (if necessary).
The possibility of asking patients with no or mild symptoms to stay at home to quarantine should also be discussed in light of hospital beds shortages.
We only hear about the lack of capacity recently with the Prime Minister’s announcement that our healthcare system is at a ‘breaking point’ in terms of ICU and non-ICU bed utilisation rates. Why isn’t this information included as part and parcel of the DG’s Covid-19 briefing and press statement?
Q6: What were the Covid-19 transmission rates in schools when there were face-to-face classes in 2020?
One of the biggest challenges faced by parents in 2020 is the shutting down of schools due to Covid-19. The Ministry of Education (MOE) decision to shut down all primary and secondary schools until the end of 2020 seems like a ‘one-size-fits-all’ approach that does not take into account variances in Covid-19 cases across districts and states.
As important, MOE has not disclosed any data or analysis with regards to transmission rates within schools.
The information which has been released by MOH tells us nothing about how children of a school-going age may have gotten the virus.
Indeed, the manner in which some data has been released by MOH and reported in the news seems misleading. For example, in a statement on June 23, 2020, the DG of Health said that one in five Covid-19 or 20 percent of patients in Malaysia is 18 years and below.
On Oct 22, the DG was reported to have said that more than 1,000 school-going children were infected with the virus since the start of the 3rd wave from Sept 20 to Oct 21. During this time, it was reported that 587 cases involved pupils aged from seven to 12 and 670 cases involved students aged 13 to 18.
These reports seem to give the indication that the students contracted Covid-19 while attending school. This will inevitably stoke unnecessary fears among parents who may have second thoughts about sending their children to school.
What do international studies and benchmarks tell us?
In an update on Oct 21, 2020, the World Health Organization (WHO) made the following conclusions among Covid-19 transmissions in schools:
- There were few outbreaks reported in schools since early 2020 and in most Covid-19 cases reported in children, the transmission occurred at home;
- More outbreaks were reported in secondary/high schools than in primary/elementary schools;
- In school outbreaks, it was more likely that the virus was introduced by adults rather than by other children; and
- School outbreaks were only high when the incidence of local/community transmission was high.
The same WHO study also recommended that schools be closed when there is no other alternative because of the negative effects of school closure, especially on marginalised children who may drop out of school and who may be deprived of school-based services such as school meals and mental health support.
In a publication on Sept 14, the WHO, Unicef and Unesco wrote that “decisions on full or partial closure or reopening should be taken at a local administrative level, based on the local level of transmission of SARS-CoV-2 and the local risk assessment, as well as how much the reopening of education settings might increase transmission in the community”.
If schools are to reopen for face-to-face classes in the recovery MCO and conditional MCO states on Jan 20, 2021, MOH and MOE have to disclose data publicly in order to convince parents that it is safe to send their kids to schools.
Q7: Housing situation for foreign workers in the security, manufacturing and construction industries?
One of the main transmission channels for the Covid-19 virus has undoubtedly been dormitories which house foreign workers who work as security guards, construction workers and factory workers.
Some of the glove manufacturers with a high number of Covid-19 cases were asked to shut down ‘in stages’ but were allowed to reopen after their workers were tested. But thus far, there has not been any concrete policy announced by the MOH or the Ministry of Human Resources to force employers to provide for less cramped accommodation for the sectors with the most number of Covid-19 cases.

There has also not been a coherent testing policy announced for the construction and manufacturing sectors. Such policies must be put in place in order to keep the Covid-19 transmission rates low, especially after MCO 2.0 is lifted.
Without proper testing and accommodation policies for these foreign workers, it is less likely that Covid-19 infection rates can be controlled after the lifting of MCO 2.0
Q8: What is the Rt Value by state, and why isn’t this figure publicly available?
MOH publishes the daily Rt value for the entire country on its Covid-19 website. This figure currently stands at 1.17. Any value above 1.0 means that the number of cases is expected to grow and any number less than 1.0 means that the virus is under control and the number of cases can be expected to decrease over time.
It would also be useful for MOH to publish daily Rt values for each state in Malaysia so that there is more clarity on which states are performing better and which states are doing worse from an infection control standpoint.
The Rt value by state can and should also be used as an indicator on when an MCO should be declared for a state and when it should be changed to a conditional MCO or a recovery MCO. For an even more targeted approach, the Rt value can be used for individual areas within a state.
The Rt value by state clearly exists since DG Noor Hisham has referred to it in one of his Facebook posts on Dec 20, 2020. Why not disclose the state by state figures on a regular basis?
Q9: How has the federal government worked with the respective state governments to fight Covid-19?
Thus far, the fight against Covid-19 seems to be one that is controlled and dictated mostly by the federal government with MOH, specifically the DG, taking the lead. There has been little coordination between the federal government and the respective state governments to join forces in the spirit of cooperation and solidarity.
Former health minister Dr Dzulkefly Ahmad, who is also the chair of the Selangor Taskforce on Covid-19 (STFC) has publicly called for more data sharing and cooperation with the MOH but so far, his calls have gone unheeded.

It is this kind of ‘silo’ mentality which has prevented Malaysia from using a ‘whole-of-government, whole-of-society’ approach to battle this pandemic. Will this kind of mentality change, now that the number of Covid-19 cases has spiked significantly, especially in the state of Selangor?
Q10: What are we doing differently now compared to March 2020?
My last and final question is simple. With nine months of experience in dealing with the Covid-19 pandemic, what lessons have we learned, and what are we doing differently in MCO 2.0 compared to the first MCO? Do the plans which have been announced give the public confidence that the MOH and also the rest of the government are capable of bringing down the Covid-19 numbers without collapsing the economy?
There is little indication that this government has learned from the experiences of the past nine months. Last-minute SOPs issued after the start of MCO 2.0, U-turns on which sectors can open, e.g. the automotive manufacturing sector and optometrists and uncertainty over school reopening are just some examples of the failure of this government to prepare for MCO 2.0. As the adage goes, “if we fail to plan, we plan to fail”.
ONG KIAN MING is Bangi MP and assistant political education director of the DAP.
The views expressed here are those of the author/contributor and do not necessarily represent the views of Malaysiakini.
RM12.50 / month
- Unlimited access to award-winning journalism
- Comment and share your opinions on all our articles
- Gift interesting stories to your friends
- Tax deductable