Covid-19: Who gets tested and how it works
KINIGUIDE | In efforts to contain the spread of Covid-19, one of the most important steps is to quickly identify those who have been infected so that they can be isolated from those who are healthy and given the appropriate medical attention.
In an interview with Vox, World Health Organisation assistant director-general Bruce Aylward said experience in China has shown that being able to quickly find and isolate cases is essential to containing the disease, even when there are many clusters of the infection.
However, the disease can be difficult to distinguish from other respiratory diseases because its symptoms are very similar.
Hence, the main method to determine whether a person is infected is to attempt to identify the virus via its genes, through a procedure known as reverse-transcription polymerase chain reaction (RT-PCR).
In this instalment of KiniGuide, we break down how the tests work, who might be eligible for testing, and what to expect.
Can I get tested?
According to the Ministry of Health’s guidelines, only people who fulfil the following criteria will be tested for Covid-19:
- People showing symptoms of fever or acute respiratory infection and have travelled to an affected country in the past 14 days. For this purpose, a person who had transited through an airport in an affected country is not considered to have travelled there.
- People who had "close contact" with a laboratory-confirmed Covid-19 case in the 14 days before the onset of symptoms, whether or not the close contact shows symptoms.
In addition, the government has a pre-existing disease surveillance programme that tests a random selection of patients with flu-like symptoms and severe acute respiratory infection, in order to keep track of trends in the diseases.
The surveillance program was expanded in February to include Covid-19 tests.
This is in order to monitor signs of sporadic cases of the disease and community transmission of the disease.

Who is a close contact?
Health Ministry guidelines list four categories of people as close contacts:
- Healthcare-related exposure, such as healthcare workers providing care for Covid-19 patients without the appropriate personal protective equipment (PPE), visitors, and patients living in the same ward as the Covid-19 patient.
- People who have worked together in close proximity or shared the same classroom environment as a Covid-19 patient.
- People who have travelled together with a Covid-19 patient by any means of transport.
- People who live in the same household with a Covid-19 patient.
Note that all of the above pertains to laboratory-confirmed Covid-19 patients, not suspected cases.
Health Ministry officers will interview patients to determine who might meet these criteria and attempt to seek them out for testing.
According to Health Ministry deputy director-general (public health) Dr Chong Chee Kong during a media engagement session on March 9, the ministry is not concerned about people becoming infected through "casual contact" with Covid-19 patients.
He said at the time that all Covid-19 patients up to that date had been in a close contact situation with another Covid-19 patient or had a travel history to an affected country.

I’m eligible for testing. Should I head straight for a clinic/hospital?
Not so fast! This is an urgent matter, but the first thing you should do is to contact the Health Ministry’s hotline as soon as possible.
They would be able to advise whether you should undergo testing and provide you with specific instructions for your case. Testing is free if you meet the testing criteria.
You may also be instructed to go to a particular healthcare facility that is equipped to screen for Covid-19 cases.
You may be directed to a designated area at the facility for screening to keep you separate from other patients and healthcare workers who don’t have the necessary PPE to handle your case. This may be a side entrance or a makeshift canopy erected outside the facility.
Calling ahead will also help healthcare workers prepare for your arrival and ensure all the necessary precautions are in place.
You may call the Health Ministry’s National Crisis Preparedness and Response Centre (CPRC) at 03-8881 0200, 03-8881 0600, or 03-8881 0700; or one of its state-level counterparts.
You may also email the national CPRC at [email protected] or use the Virtual Health Advisory Portal.
The latter is an online service and is a collaboration between the ministry and DoctorOnCall. There is also an online assessment tool that can help you assess the probability that you may be having a Covid-19 infection.
You may also contact any of the above hotlines with other questions about Covid-19. It is operated from 8am to 5pm.

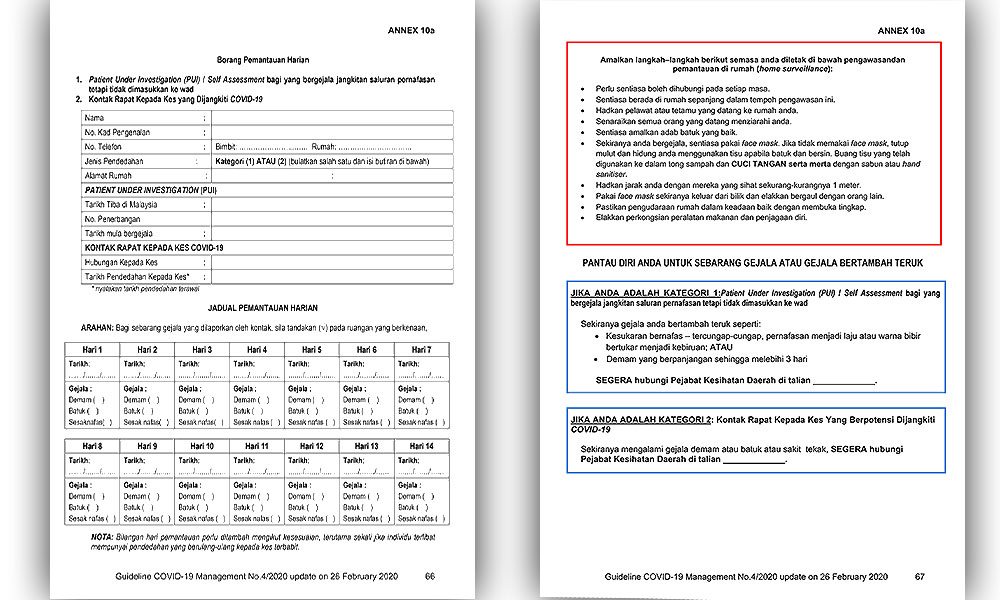
What happens after I get tested?
If you are showing symptoms or is otherwise unwell, you will be admitted to a ward pending your results. You may also be warded if your home environment is not suitable for quarantine.
If you don’t have symptoms and your home environment is suitable for quarantine, then you will be given instructions on how to quarantine yourself for 14 days from the date you were last exposed to a Covid-19 patient.
A health official will check on you daily and monitor your symptoms.
It is mandatory that you follow these instructions. Failure to comply would mean you are a public health risk and may result in legal action.
According to Health Ministry guidelines, examples of cases that are suitable for home quarantine are where the patient has access to a separate bedroom (preferably with an en-suite bathroom), has access to daily necessities and private transport, and able to stay away from high-risk household members such as the elderly.
I’m not eligible for testing but want to get tested anyway. What can I do?
Public healthcare facilities may refuse to test you to focus on providing care to those who need it.
For a fee, you may seek testing from private healthcare providers instead.
Health Ministry director-general Dr Noor Hisham Abdullah (photo) said 11 companies have been provided with the necessary training and quality checks by the ministry to conduct the sampling and tests.
You may also arrange for a medical team to be sent to your home to conduct sampling there.

What do they need for the test? Blood?
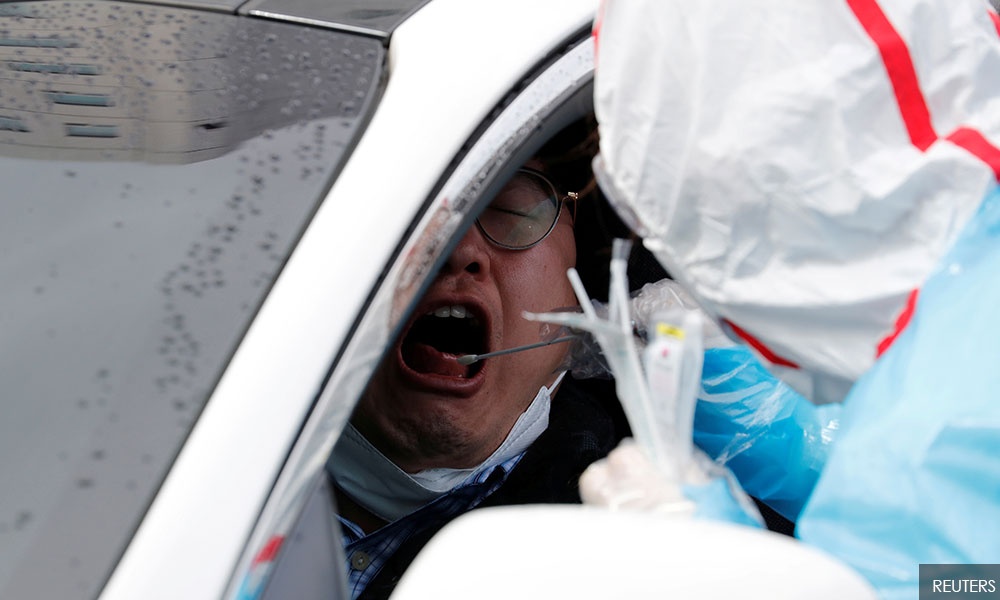
No, the test usually calls for swab samples taken from the nose and the mouth instead.
The instrument comprises a small polyester swab attached to a long shaft. Medical personnel will insert it deep into your mouth and/or nose, and scrape the swab against the back of your throat or nose (a part known as the nasopharynx).
The depth is several inches, approximately the same distance from the mouth or nose to your ear. Those who have undergone the procedure generally describe it as extremely unpleasant but not painful.
The swab will then be sent for testing.
For patients already showing symptoms, other methods may be used especially if the patient is very ill, such as testing the phlegm that may be produced by the patient or have lung washing samples taken.
In the latter case - known as a bronchoalveolar lavage - a tube is inserted through the mouth and nose into the lungs. A fluid is then squirted into a small part of the lungs through the tube and then collected for testing.
What happens to the samples?
The first step is to extract the virus’ genetic material (RNA) from the sample collected.
An enzyme known as reverse transcriptase is then used to convert the virus’ genetic information into DNA, which can then be repeatedly copied many times so that even small amounts of the material is readily detectable.
The process of DNA amplification is known as polymerase chain reaction (PCR), and its use in combination with reverse transcription (RT) is what gives rise to the name RT-PCR.

The reaction mixture also contains molecular "probes" that are specially designed to attach themselves to target genetic sequences that are unique to the virus that causes Covid-19.
The probe contains a fluorescent dye that is in an inactive form. After attaching itself to the target sequences, the dye is cut loose in the next round of DNA amplification and becomes activated.
A sensor records the results, and the amount of fluorescent light detected can be used to calculate the amount of viral RNA originally present.
That’s a lot of work. How good is this test?
The test was developed in-house by the Institute of Medical Research (IMR) in Kuala Lumpur on Jan 11, based on genetic data published by scientists in China on the same day.
It costs RM700 to test each patient.
In a statement, Noor Hisham said the test could take up to 24 hours to yield results but usually, the results are ready much earlier.
It is not publicly known how reliable is the test developed by IMR but in general, RT-PCR tests are regarded as extremely unlikely to produce "false positive" results.
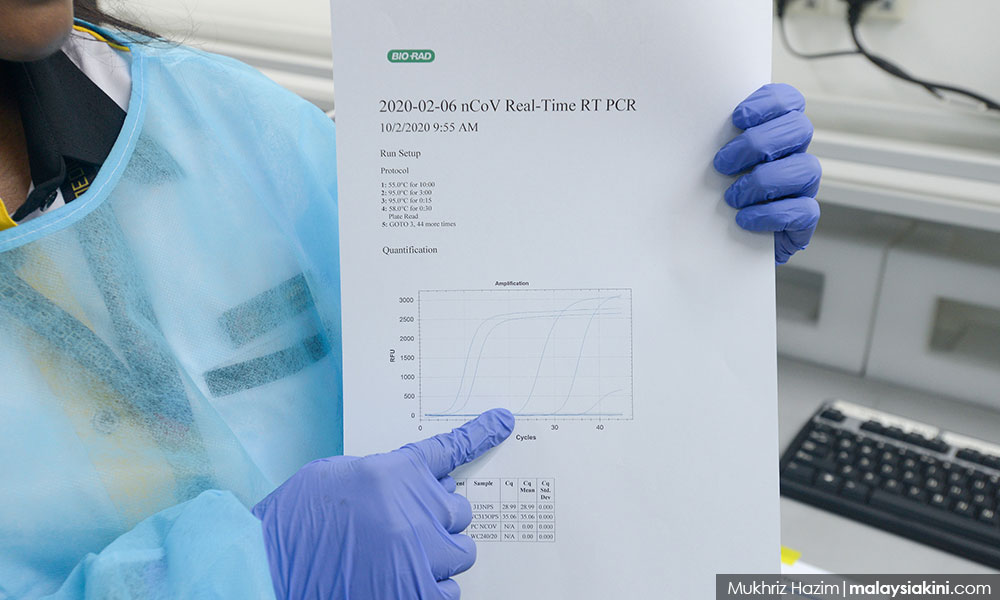
In addition, a joint report by the WHO and China last month said preliminary data showed that RT-PCR tests can detect the virus one or two days before symptoms appear.
Conversely, however, a single negative test result is not regarded as conclusive.
To mitigate "false negatives", Health Ministry guidelines require someone who has tested negative to be re-tested.
What happens if I test positive?
If you are not already admitted to a hospital ward, you will be.
There are 26 public hospitals and one university hospital that are equipped and trained to handle Covid-19 cases.
Health officials will begin tracing your close contacts, and it is essential that you provide full cooperation to this process to help curb further spreading of the disease.
What happens if I test negative?
If you were warded, you need to test negative twice in a row to be eligible for discharge.
If you were in home quarantine, you will need to remain in quarantine until the end of the 14-day period.
You will be tested for a second time on the 13th day and will be released on the 14th day if the results are negative.
How much testing is being done?
The Health Ministry provides daily updates on the number of cases tested on its website.
As of March 22 at 5pm, 15,196 cases have been tested. Of this, 1,306 (8.6 percent) tested positive, 9,969 (65.6 percent) tested negative, and 3,921 (23.8 percent) are still pending.
If the tests that are still pending are excluded, the proportion of positive versus negative cases is 12.3 percent and 87.7 percent respectively.
As noted above, each case would have been tested more than once.
Noor Hisham told a press conference on March 22 that Malaysia aims to test 16,000 cases per day, and this is being done in 18 laboratories all over the country.
At present, the country is able to conduct up to 4,500 tests a day. The government plans to increase this to 7,000 by next week and 16,000 by April.
Is RT-PCR the only test being done?
No. For patients with symptoms, Health Ministry guidelines required blood serum samples to be collected and sent to the IMR for testing.
The serum sample is to be collected between five and eight days after admission to a hospital or upon discharge.
The purpose of this test is not specified in the guidelines but in general, such tests are used to detect the presence of antibodies produced by a patient’s body to fight off a Covid-19 infection.
This may be used to monitor a patient’s condition or corroborate with earlier RT-PCR test results to confirm that an infection had indeed taken place.

I’ve seen small test kits being sold on the market. Can I use that to test myself at home?
Firstly, you should consult a medical professional on whether the test is suitable for your case and for the interpretation of those results.
The findings of such tests may need to be corroborated with other findings to ensure that it is valid.
This is because these tests work by detecting antibodies produced by the body in response to a Covid-19 infection, in order to fight off the disease.
It could take weeks to build up enough antibodies to be detected and by then, the body may have already been cleared of the virus. Other people may have already been infected over the course of the disease.
In other words, antibody-based tests can detect a previous infection. However, it may miss one that is ongoing and contagious.
In contrast, the RT-PCR test can detect the presence of the virus itself and thus, useful for diagnosing infected persons and quickly isolating them.
Meanwhile, Noor Hisham told reporters when met on March 22 that the suitability of such tests depends on what you are trying to find out from the test.
“As I’ve said, it depends on the reason why you measure (the antibodies). If you measure for antibodies, you can - for example - determine whether there is a class of people with herd immunity because everyone has that antibody.
“So, you can measure that. It depends on the test, and what you want to do,” he said.
This instalment of KiniGuide was compiled by KOH JUN LIN.
Keep up with the latest information on the outbreak in the country with Malaysiakini's free Covid-19 tracker.
RM12.50 / month
- Unlimited access to award-winning journalism
- Comment and share your opinions on all our articles
- Gift interesting stories to your friends
- Tax deductable